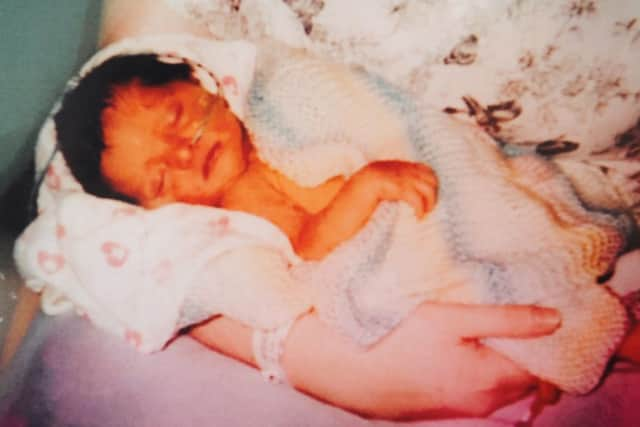
Tragic baby Ava died after treatment which was meant to save her life


Tragic Ava Marie Calvert appeared a healthy little girl when she came into the world on June 17, last year.
But she was just a few hours into her life, when doctors at Sunderland Royal Hospital diagnosed low blood sugar and she was given routine treatment to increase her glucose levels.


Advertisement
Hide AdAdvertisement
Hide AdHowever, the decision to give this via a long line caused a massive blood clot, which remained undetected until after her death, an inquest heard.
The clot had completely blocked her pulmonary artery and caused her rapid death, with a senior medic describing the case as “fantastically rare.”
After rushing to the hospital in the early hours on June 29, Ava’s parents Jade Hutchinson and Jason Calvert, of Alexandra Park, Sunderland, were horrified to find that doctors had switched off their daughter’s life support without consulting them first.
The youngster was less than a fortnight old when she was pronounced dead in her mother’s arms at 6am.

Advertisement
Hide AdAdvertisement
Hide AdTo compound the family’s anguish, they later received an ‘event of death’ report through the post from the hospital - something that should never have happened - while Miss Hutchinson continued to receive texts and phone calls from the breastfeeding service in the following weeks.
Sunderland’s senior coroner Derek Winter recorded a conclusion of misadventure, meaning that Ava died as a result of a lawful act.
But Mr Winter added that he would be writing to hospital bosses, about concerns with record keeping and communication, and to the Chief Medical Officer to raise awareness of the case so doctors can be alerted to any future instances.
Pathologist Dr Srinivas Annavarapu, who carried out a post mortem on Ava recorded the cause of death as acute cardio-respiratory failure, caused by the blood clot, and as a result of the insertion of the central line.


Advertisement
Hide AdAdvertisement
Hide AdAva’s hyperinsulism – or excessive insulin production – which caused her low blood sugar, was listed as a contributory factor. The condition is understood to affect just one in 50,000 babies.
A pulmonary blood clot in an infant has never before been described in medical literature, the inquest heard.
Consultant paediatrician Dr Josephine Flowers said that not correcting blood sugar causes seizures, coma and eventually, death.
“The treatment we gave her contributed to her death, but without that dextrose, without this central catheter, we perhaps wouldn’t be able to keep her alive in the first place,” she said.

Advertisement
Hide AdAdvertisement
Hide AdConsultant Neonatologist Dr Imran Ahmed said an ultrasound of Ava’s heart on June 24, did not reveal a blood clot.
“We wouldn’t have been actively looking for that because, as we’ve heard, it’s not something we would have been thinking about,” he said.
Ava was born by emergency C-section because Miss Hutchinson suffered from dangerously high blood pressure prior to the birth. As a result, she herself spent 28 hours in the high dependency unit, before visiting her daughter as often as possible when as she recovered. Giving evidence, Miss Hutchinson said she had numerous concerns about Ava’s care. She said she had found her lying in her own vomit and with her feeding tube in her ear.
It had also been revealed that a student nurse inserted the central catheter, after two failed attempts by qualified colleagues. She also arrived at the hospital to find her daughter had been moved between units without any records being kept as to where she was.
Advertisement
Hide AdAdvertisement
Hide AdMiss Hutchinson spoke about the day before Ava deteriorated so catastrophically.
“They said they were going to look to me managing her blood sugar at home,” she told the inquest. “I was under the impression that, because we were starting this process she was going home. Everything was going great. I was quite happy.”
But at 3.30am the following morning the couple were awoken by police at their front door, telling them they needed to go immediately to the hospital. There they were met by consultant neonatologist Dr Ruppa Geethanath.
“Dr Geethanath explained Ava was in a critical condition, that she may not pull through, and at this point we had to prepare for the worst,” Miss Hutchinson said.
Advertisement
Hide AdAdvertisement
Hide Ad“When Dr Geethanath said he didn’t know what was wrong with her that didn’t instil any confidence.”
Ava was christened in the hospital, but though her parents begged doctors not to turn off her life support, they went ahead with it.
“I said please don’t disconnect her,” Miss Hutchinson said. “I wasn’t given the option or told about the situation. I didn’t know anything about Dr Geethanath turning her off.”
Dr Geethanath said: “I did my best to explain to the parents, but because it happened so suddenly, I myself didn’t know why this happened in the first place.”
Advertisement
Hide AdAdvertisement
Hide AdHe added: “We struggled with Ava for close to three hours. We did everything we could. I did tell the parents that she wouldn’t survive. Her heart stopped while she was on the ventilator.”
Independent expert Professor Andrew Whitelaw told the inquest: “A baby dying of a thromboembolism is a fantastically rare event.
“I can’t find a description of what happened to Ava, that’s how rare this is.
“I think it would be worth reporting this in the medical literature because I think it’s worth notifying the neonatal community that this has happened to Ava.”
Advertisement
Hide AdAdvertisement
Hide AdOn concluding the hearing, Mr Winter said, that while he was not critical of anyone involved, he would write a report to the Chief Medical Officer and the Care Quality Commission under Regulation 28, to prevent future deaths.
He said: “So that there is awareness of the dangers of clots occurring and that they may occur so that doctors can be alerted, that they can as a result look for something that may prevent the terrible time that the family have had.
Mr Winter added that he will also write the chief executive of Sunderland Royal Hospital, about concerns with record keeping and communication.
“Ava’s death can have the effect of undermining confidence in the care and treatment of a patient,” he said. “Miss Henderson should never have had that death event report in the post, there was communication about breast feeding. It is important to ensure that does not happen.
Advertisement
Hide AdAdvertisement
Hide Ad“I would also like the chief executive to look at how communication can be improved around end of life care.”
A spokeswoman for City Hospitals Sunderland said: “This was an extremely sad case which found that unfortunately the death of Ava Marie could not have been prevented.
“We would like to offer our deepest sympathies to Ava Marie’s family at what has been, and continues to be, a very distressing time for them.”